Becoming a heart mom: Birth edition
December 17, 2021, the day I became a mom of three, the day my heart warrior arrived, was the best and worst day of my life. This is a day I’ll never forget. Without a doubt, it was the most emotionally charged day of my life.
Things did not go according to plan, which is of course common when it comes to birth and babies. Especially in these medically complex situations, but it was beyond what I imagined as a possible scenario.
There was so much stress throughout this pregnancy. We were so excited to meet our baby girl, trepidly excited. With her Congenital Heart Defects (CHDs) she was safer inside than outside.
Labor as a heart mom
Once my baby was diagnosed with an AV canal defect, I earned a high-risk flag. I also had a Velamentous Cord Insertion (VCI) and low-PAPP-A which further put us in the high-risk category. Despite these complications, after much discussion, my team was okay with my preferred plan to go into labor spontaneously and birth vaginally.
My water broke at home while I was sleeping. At first, I wasn’t certain this was it because it was only a tiny bit, and with my previous pregnancies, this didn’t happen. So I waited a bit to see if it would continue.
Water kept coming in small gushes, and my contractions started to pick up with regularity. I called my midwife to share what happened and planned to head to the hospital. I would have labored at home longer until my contractions intensified if the pregnancy was low risk. But because of all the risk factors, it made sense to head to the hospital early.
They wanted to monitor the baby continuously to make sure she wasn’t in distress throughout labor. And they needed to monitor me as well to make sure I didn’t have any excessive bleeding issues because of the VCI.
Based on my first two labor experiences, I knew I would manage my labor better by standing. Unfortunately, when standing and trying to move through my contractions, my baby’s heart rate would drop. After they saw this pattern repeating, they had me stay in bed for a period. Agony! Finally, they figured out a solution with a support belt thing which kept the monitors on better even when standing (and I think it was more the monitors slipping than her heart rate).
Birthing as a heart mom
Similar to my previous two labors, early labor was a bit slow. Once things got moving though, it went quickly. I planned a natural, drug-free birth and questioned my sanity during the transition, but ultimately succeeded.
The NICU team was in the room for the birth ready to assess her and take any quick action if necessary. Though we were only at a level 2 NICU hospital, as she was expected to be okay at birth. (US hospital NICUs are categorized by levels 1-4 and correspond to how much support they can provide neonates.)
Meeting my heart warrior
She came out looking pretty purple but “pinked up nicely” fairly quickly, except for her hands and feet. I immediately got to bring her to my chest and marveled at the fact that she was really here. I was allowed to hold her for maybe a minute.
Extra monitoring for a heart mom’s birth
Before I knew it, our bliss was sliced by a request to cut the cord and take her for assessments. Becoming a heart mom is a heart-wrenching experience. Nothing prepares you for when they take your baby from you right after birth. While essential, it’s anything but easy. It was so painful, physically and emotionally. And the NICU team only had to take her across the room.
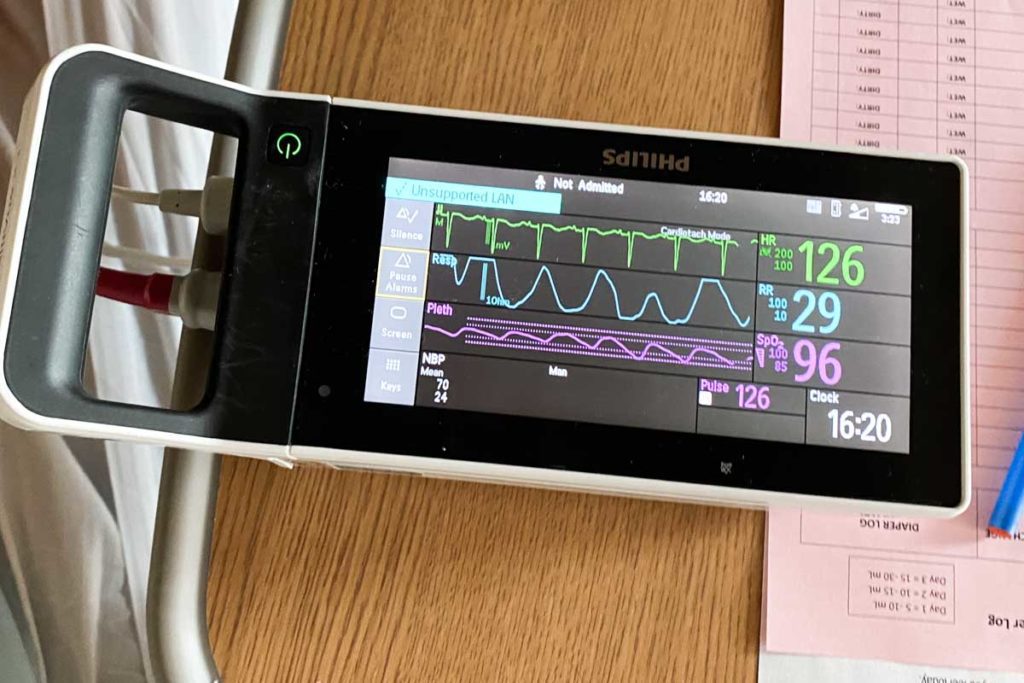
The neonatologist had to assess her more closely and set up her monitors. We got to keep her in the room with us, she had to have oxygen, pulse, and heart monitors on. But otherwise, we were able to resume our long-awaited meeting, a slightly interrupted and untraditional, but amazingly sweet golden hour.
We had to keep a beeping monitor machine close to her, but we were able to move it around. Her vitals and oxygen saturations were good, and she was maintaining well on room air. She looked so good and was acting like a typical newborn baby. There were no external signs of a congenital heart defect. I was able to nurse her, and she latched beautifully.
It was such a difficult pregnancy – physically and emotionally – the post-birth endorphin rush and relief that she was doing well were euphoric. Everything was good up to this point and we were riding the high.

Extra newborn tests at birth for a heart mom
An hour or so after birth, they took her out of the room to the NICU for her echocardiogram. We knew about this ahead of time and it was important, actually essential, and life-saving for her. Still, letting my newborn baby go was harder than I imagined.
They said they would return her to us in 45-60 minutes, and agonizingly they took longer. It was so difficult to not let our minds wander to the negative, but she was back in our arms around 90 minutes later. We continued enjoying the heavenly newborn snuggles.

Subscribe to stay closest to heart parent guides, updates, stories and other CHD information.
By subscribing to our newsletter you agree to our Terms and Conditions and Privacy Policy.
An unexpected discovery, more heart problems
A few hours later, things took a turn. It still aches as I recall the turn of events.
The neonatologist returned to discuss the echo findings. Her face said it all and she barely began before my first tear fell. “Her heart is looking more complex than originally diagnosed…” And then I couldn’t hold back the flood.
I held and nursed baby girl tears flowing in bewilderment. How can this seemingly perfect miracle be so critically ill?
Abruptly the doctor started, “did you pick a surgeon yet?” No, I hadn’t, we were supposed to have more time. How do you decide? And she pressed the importance of making a decision now.
This hospital did not have the capabilities and specialists to determine the best course of action. Their job was to keep her stable until she could be transferred.
The NICU team conferred with the hospital’s cardiologist, however, this was not a pediatric-specific one. In our denial of this new reality, we insisted on including our pediatric cardiologist in the discussion. Frustratingly she was unavailable, but at least another member of the practice was.
Bleakly we grew to accept the change in direction after discussing it with the pediatric cardiologist. We were looking at the best-case scenario of being transferred to a children’s hospital for a more thorough evaluation, and medicine and otherwise being able to go home and wait on any further interventions.
However, this sounded unlikely. Instead, we were likely looking at a transfer and a much earlier heart procedure or surgery.
A new direction, NICU and transfer to Children’s
We could no longer keep her in the room with us. She had to move to the NICU immediately for constant monitoring and IV access.
They would need to repeat the echo to track her Patent Ductus Arteriosus (PDA). She would need more testing and consultations with cardiology to determine her exact anatomy and defects, and the best plan. And she would need to be transferred to a children’s hospital with pediatric cardiac surgical capabilities.


An emotional rollercoaster doesn’t seem to even begin to cover the extremity of emotions. Gutted. Shocked. Heartbroken. Denial.
This wasn’t supposed to happen. We were supposed to bring her home. I was prepared for her to possibly spend a couple of days in the NICU.
Christmas was only a week away. We were supposed to snuggle up on the couch at home with our brand-new baby and watch as our 6 and 4-year-olds delight in the buildup to Christmas.
I knew her diagnosis could change at birth, but everyone seemed confident that her diagnosis was clear. I had so many appointments and tests, and we met with two world-class surgeons who reviewed the echos, so I felt confident in that and had moved past the worry that things could change at birth.
We had discussions with various doctors and picked a surgeon and hospital. Then we had to sign transfer consent forms, death was listed as 1 of 2 risk possibilities. Next, we pushed to get me discharged.
At 24 hours old, Isa was taken by ambulance an hour and a half away to the Children’s Hospital Los Angeles. We left the hospital without our baby, went home, saw the boys and my parents, packed a bag for an undetermined amount of time, and headed to LA.
Read more: A real-life nightmare with our 1-day-old newborn
I knew a heart mom birth wasn’t going to be easy, still, this was not the birth date I imagined for my baby girl.
This is CHD (Congenital Heart Disease).